Osteoporosis: Early Warning Signs, Causes, and Treatment
Our bones are the silent heroes of our bodies. They not only enable mobility, but also protect our vital organs and store essential minerals. Unfortunately, with age, bones can lose their strength, often without any warning. This is what usually happens in the case of osteoporosis, also known as a “silent disease” that weakens bones and frequently remains unnoticed until a sudden fracture occurs. Living with the risk of fragile bones can be daunting, especially when there are no obvious symptoms to signal a problem. That’s why understanding osteoporosis and recognising the early signs are so important. To help, in this blog, we will discuss what osteoporosis is, its symptoms, risk factors, and causes, along with available treatment and prevention strategies to help maintain strong, healthy bones.
Table of Contents
ToggleWhat is Osteoporosis?
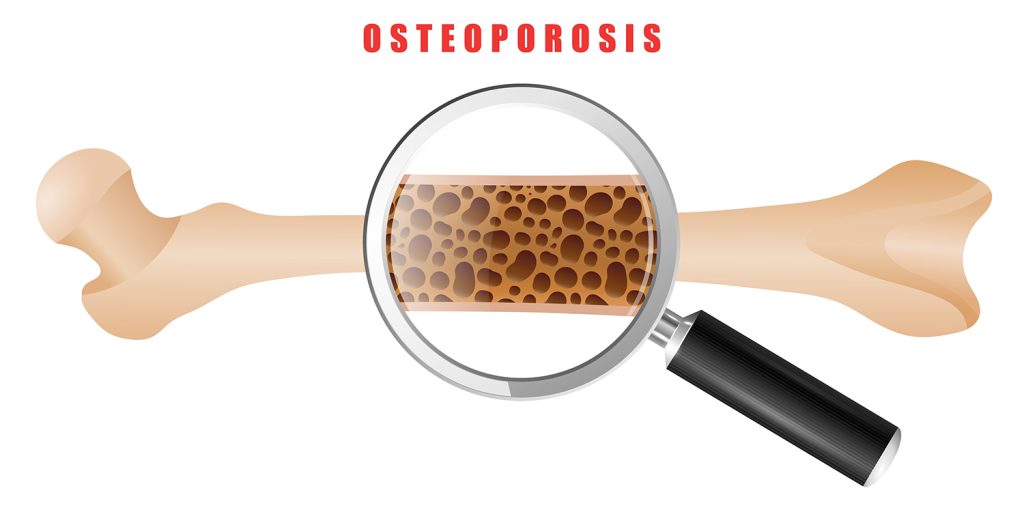
Osteoporosis is a progressive bone disease characterised by a decrease in bone mass and density, leading to fragile bones that are more prone to fractures. The term “osteoporosis” literally means “porous bones,” reflecting the condition’s impact on bone structure. Healthy bones have a dense, honeycomb-like structure, but in osteoporosis, the spaces within the bone become larger, weakening its strength and integrity.
This condition develops when the body either loses too much bone, makes too little bone, or both. As bones become less dense, even minor falls or simple actions such as bending or coughing can result in fractures, particularly in the hip, spine, or wrist. Osteoporosis affects millions worldwide, particularly postmenopausal women and older adults, but it can also impact men and younger individuals under certain conditions.
Understanding osteoporosis is the first step towards recognising its risks and taking proactive measures to protect bone health.
Read more-What is a Tennis Elbow: Causes, Symptoms, Treatments, and Prevention
What are the Different Types of Osteoporosis?
Osteoporosis isn’t a one-size-fits-all condition. It can be classified into different types based on its cause and the underlying factors that contribute to bone loss. Understanding these types can help in identifying risks and tailoring appropriate treatment and prevention strategies.
1. Primary Osteoporosis
Primary osteoporosis is the most common form and occurs as a result of the natural ageing process or hormonal changes, particularly in women after menopause.
- Type I (Postmenopausal Osteoporosis): This type typically affects women after menopause due to a significant drop in oestrogen levels — a hormone crucial for maintaining bone density. It often leads to fractures in the wrist or spine.
- Type II (Senile Osteoporosis): Also known as age-related osteoporosis, this type generally affects both men and women over the age of 70. It results from a natural decline in bone formation and calcium absorption, leading to fractures, particularly in the hip and spine.
2. Secondary Osteoporosis
Secondary osteoporosis occurs as a result of specific medical conditions, medications, or lifestyle factors that contribute to bone loss.
- Medical Conditions: Disorders such as hyperthyroidism, chronic kidney disease, rheumatoid arthritis, and gastrointestinal diseases that affect nutrient absorption can lead to bone weakening.
- Medications: Long-term use of certain medications, like corticosteroids, anticonvulsants, and some cancer treatments, can negatively impact bone health.
- Lifestyle Factors: Poor nutrition, excessive alcohol consumption, smoking, and a sedentary lifestyle can all increase the risk of developing secondary osteoporosis.
Understanding the type of osteoporosis is essential in determining the most effective treatment plan and preventive measures.
What are the Early Warning Signs and Symptoms of Osteoporosis?
Osteoporosis is often called the “silent disease” because it progresses without obvious symptoms until a bone fracture occurs. However, there are early warning signs that can help in identifying the condition before it leads to serious complications.
Early Warning Signs of Osteoporosis
- Receding Gums: Bone loss in the jaw can cause gums to recede, which may be an early indicator of osteoporosis.
- Weakened Grip Strength: A noticeable decrease in grip strength can signal weakening bones.
- Brittle Nails: Nails that break or chip easily may be a subtle sign of reduced bone health.
- Decreased Bone Density on Tests: Routine bone density scans (DEXA scans) can reveal lower-than-normal bone density, even before symptoms appear.
Common Symptoms in Advanced Stages
As osteoporosis progresses, more noticeable symptoms may develop, often after significant bone loss has occurred.
- Frequent Fractures: Bones become so fragile that fractures occur easily, even from minor falls or everyday activities like bending or lifting. Common fracture sites include the hips, wrists, and spine.
- Loss of Height: A noticeable reduction in height over time can result from compression fractures in the spine.
- Stooped Posture: Spinal fractures may cause a stooped or hunched posture, known as kyphosis.
- Chronic Back Pain: Compression fractures in the vertebrae can lead to persistent back pain.
Recognising these early warning signs and symptoms can help in diagnosing osteoporosis before significant damage occurs, allowing for timely intervention and treatment.
Read more-Inflammatory Arthritis Explained: From Symptoms to Management
What Causes Osteoporosis?
Osteoporosis develops when the body loses too much bone, makes too little bone, or both, leading to weakened bones that are prone to fractures. Several factors can contribute to this imbalance in bone formation and resorption.
Natural Bone Loss with Age
Bone is living tissue that constantly undergoes renewal. In younger years, bone formation outpaces bone loss, leading to stronger, denser bones. However, as people age, this process slows down, and bone loss begins to exceed bone formation. After the age of 30, bone mass gradually declines, increasing the risk of osteoporosis.
Hormonal Changes
- Oestrogen Deficiency: In women, a sharp decline in oestrogen levels after menopause accelerates bone loss, making postmenopausal women particularly vulnerable to osteoporosis.
- Testosterone Deficiency: Men experience a more gradual decline in testosterone, but low levels can still contribute to reduced bone density.
- Thyroid Imbalance: Overactive thyroid (hyperthyroidism) can speed up bone loss, leading to weakened bones.
Nutritional Deficiencies
- Calcium Deficiency: Calcium is a key component of bone structure. Inadequate calcium intake over time leads to lower bone density and an increased risk of fractures.
- Vitamin D Deficiency: Vitamin D is essential for calcium absorption. Without enough vitamin D, bones cannot properly absorb calcium, leading to bone loss.
- Protein Deficiency: Protein is important for bone health, and insufficient intake can negatively impact bone strength.
Medical Conditions and Medications
- Chronic Illnesses: Conditions such as rheumatoid arthritis, celiac disease, inflammatory bowel disease, and chronic kidney disease can impair bone health.
- Certain Medications: Long-term use of corticosteroids, anti-seizure drugs, and some cancer treatments can interfere with bone-building processes, leading to osteoporosis.
- Gastrointestinal Disorders: Diseases that affect nutrient absorption, such as Crohn’s disease or celiac disease, can result in deficiencies critical for bone health.
Lifestyle Factors
- Lack of Physical Activity: A sedentary lifestyle, especially without weight-bearing exercises, can lead to bone loss over time.
- Smoking and Alcohol Consumption: Smoking impairs calcium absorption and reduces bone mass, while excessive alcohol intake interferes with the body’s ability to build strong bones.
- Poor Diet: Diets low in essential nutrients like calcium, vitamin D, and magnesium can weaken bones over time.
Read more-Everything You Should Know About Septic Arthritis
How is Osteoporosis Diagnosed?
Diagnosing osteoporosis early is essential to prevent fractures and manage bone health effectively. Since the condition often develops silently without noticeable symptoms, regular screenings and diagnostic tests play a crucial role in detecting bone loss before it leads to complications.
1. Bone Density Test (DEXA Scan)
The most common and reliable method for diagnosing osteoporosis is the Dual-Energy X-ray Absorptiometry (DEXA or DXA) scan. This non-invasive test measures bone mineral density (BMD) at critical areas, such as the spine, hip, and wrist, which are most prone to fractures.
- T-score Interpretation:
- Normal Bone Density: T-score of -1.0 or higher
- Osteopenia (Low Bone Mass): T-score between -1.0 and -2.5
- Osteoporosis: T-score of -2.5 or lower
The lower the T-score, the weaker the bone density and the higher the risk of fractures.
2. Additional Diagnostic Tests
- X-rays: Although not sensitive enough to detect early bone loss, X-rays can reveal fractures or spinal deformities associated with advanced osteoporosis.
- Quantitative Computed Tomography (QCT): This imaging technique provides a 3D assessment of bone density and is sometimes used when more detailed information is needed.
- Ultrasound: Peripheral ultrasound tests (commonly on the heel) can give a general idea of bone density but are not as precise as DEXA scans.
3. Laboratory Tests
To identify underlying causes of bone loss or rule out secondary osteoporosis, doctors may recommend blood and urine tests to assess:
- Calcium and Vitamin D levels
- Thyroid and parathyroid hormone levels
- Markers of bone turnover
- Kidney and liver function tests
These tests help determine if hormonal imbalances, nutritional deficiencies, or other health issues are contributing to decreased bone density.
Who Should Get Tested?
While osteoporosis is often associated with older adults, it’s important to recognise that younger individuals can also be at risk. Lifestyle factors, medical conditions, and certain medications can lead to weakened bones even at a younger age, making early screening crucial for more than just the elderly. Bone density testing is recommended for:
- Women aged 65 and older and men aged 70 and older
- Postmenopausal women under 65 with risk factors for bone loss
- Adults of any age who have experienced fractures after age 50
- Younger individuals with risk factors such as family history, eating disorders, or chronic conditions like rheumatoid arthritis
- Individuals taking medications that affect bone health, such as corticosteroids
Early diagnosis through regular screenings allows for timely intervention, helping to strengthen bones, prevent fractures, and improve long-term bone health — no matter your age.
What are the Treatment Options for Osteoporosis?
Osteoporosis treatment focuses on strengthening bones, preventing fractures, and slowing or stopping bone loss. A combination of medications, lifestyle changes, and supportive therapies can help manage the condition effectively.
1. Medications for Osteoporosis
Several medications are available to help strengthen bones and reduce fracture risk:
- Bisphosphonates: These are the most commonly prescribed drugs for osteoporosis. They slow bone loss and may even increase bone density. Examples include alendronate, ibandronate, risedronate, and zoledronic acid.
- Selective Estrogen Receptor Modulators (SERMs): Medications like raloxifene mimic oestrogen’s bone-protective effects, reducing the risk of spine fractures, especially in postmenopausal women.
- Hormone Replacement Therapy (HRT): For postmenopausal women, oestrogen therapy can help maintain bone density, though it’s typically used cautiously due to associated risks.
- Parathyroid Hormone Analogues: Drugs like teriparatide and abaloparatide stimulate new bone formation and are often used in severe cases.
- RANK Ligand Inhibitors: Denosumab is an injectable medication that slows bone loss and reduces fracture risk by blocking a protein involved in bone resorption.
- Calcitonin: Though less commonly used today, this hormone helps regulate calcium levels and can provide pain relief from spinal fractures.
2. Lifestyle Modifications
Adopting certain lifestyle changes can support bone health and complement medical treatments:
Nutrition
- Calcium: Adults aged 50 and older should aim for 1,200 mg of calcium daily through diet and supplements if needed.
- Vitamin D: Essential for calcium absorption, most adults require 800–1,000 IU daily, with higher doses for those deficient.
- Protein, magnesium, and vitamin K also contribute to bone strength.
Exercise
- Weight-bearing activities like walking, dancing, or jogging help build bone density.
- Resistance training strengthens muscles and bones.
- Balance and flexibility exercises like yoga or tai chi reduce the risk of falls.
Fall Prevention
- Use handrails, remove tripping hazards, and ensure adequate lighting at home to prevent falls.
- Vision and hearing checks can also help maintain balance.
3. Managing Pain and Fractures
- Pain Management: Over-the-counter pain relievers, such as acetaminophen or NSAIDs, may help with pain caused by fractures.
- Physical Therapy: Tailored exercise programs can improve strength, balance, and posture, reducing the risk of future fractures.
- Surgical Intervention: In cases of severe fractures, surgical options like vertebroplasty or kyphoplasty may be considered to stabilise bones and relieve pain.
Osteoporosis treatment is most effective when tailored to an individual’s needs, combining medications with lifestyle strategies to maintain and improve bone health.
Read more- Frozen Shoulder: Causes, Symptoms, and Treatments
How can Osteoporosis be Prevented and Managed?
While osteoporosis can’t always be entirely prevented, adopting proactive measures can significantly reduce the risk of developing the condition and help manage it effectively in those already diagnosed. Prevention and management focus on strengthening bones, minimising bone loss, and reducing the risk of fractures.
Nutritional Strategies for Bone Health
- Calcium-Rich Diet: Calcium is essential for strong bones. Adults should aim for 1,000–1,200 mg daily through sources like dairy products, leafy greens, almonds, and fortified foods.
- Vitamin D Intake: Vitamin D helps the body absorb calcium effectively. Natural sunlight exposure, fortified foods, and supplements (typically 800–1,000 IU daily) are good sources.
- Bone-Boosting Nutrients: Include foods rich in magnesium, vitamin K, zinc, and protein, all of which play vital roles in bone health.
Physical Activity and Exercise
Regular physical activity is crucial for maintaining bone strength and improving balance to prevent falls.
- Weight-Bearing Exercises: Activities like walking, jogging, dancing, or climbing stairs encourage bone formation and help maintain density.
- Strength Training: Resistance exercises, such as lifting weights or using resistance bands, strengthen muscles and bones.
- Balance and Flexibility Training: Yoga, tai chi, and balance-focused exercises improve coordination, reducing the risk of falls.
Healthy Lifestyle Choices
- Avoid Smoking: Smoking accelerates bone loss and reduces the body’s ability to absorb calcium.
- Limit Alcohol Consumption: Excessive alcohol can weaken bones and impair balance, increasing fracture risks.
- Maintain a Healthy Weight: Being underweight can increase the risk of bone loss, while obesity can strain the skeleton and raise fracture risks.
Regular Screenings and Monitoring
- Bone Density Tests: Regular DEXA scans help monitor bone health and detect osteoporosis early, especially in individuals over 65 or those with risk factors.
- Routine Health Check-ups: Monitoring calcium, vitamin D levels, and bone turnover markers can guide dietary and treatment decisions.
Managing Osteoporosis Effectively
For those already diagnosed with osteoporosis, combining medications with lifestyle changes offers the best approach to managing the disease.
- Follow Treatment Plans: Consistently taking prescribed medications helps slow bone loss and strengthen bones.
- Physical Therapy: Targeted exercise programs improve strength, balance, and flexibility, lowering fracture risks.
- Pain and Fracture Management: Addressing pain from fractures and focusing on rehabilitation supports better long-term outcomes.
By focusing on prevention and early management, individuals can maintain stronger bones, lower their fracture risk, and enjoy a better quality of life, even with osteoporosis.
What are the Potential Complications of Osteoporosis?
Osteoporosis can lead to several complications, especially if left undiagnosed or untreated. These complications can significantly impact mobility, independence, and overall quality of life. Understanding these risks can help emphasise the importance of early detection and proactive management.
Bone Fractures
Fractures are the most common and serious complication of osteoporosis. Weakened bones are more prone to breaking, often from minor falls or even simple movements like bending or coughing.
- Hip Fractures: These are among the most severe complications, often requiring surgery and long-term rehabilitation. Hip fractures can lead to significant loss of mobility and independence.
- Spinal Compression Fractures: Osteoporosis can cause the vertebrae in the spine to collapse or compress, leading to chronic pain, height loss, and a stooped posture (kyphosis).
- Wrist and Forearm Fractures: Falls onto an outstretched hand frequently result in wrist fractures in individuals with osteoporosis.
Chronic Pain
Spinal fractures, in particular, can lead to long-term back pain and discomfort. The collapse of vertebrae puts pressure on surrounding muscles and nerves, contributing to persistent pain that can affect daily activities.
Reduced Mobility and Independence
Fractures, especially in the hip or spine, can significantly impair mobility. Many individuals experience difficulty walking, standing, or performing everyday tasks. In severe cases, osteoporosis-related fractures can lead to permanent disability or the need for long-term care.
Postural Changes
Multiple spinal fractures can cause a noticeable curvature of the spine, known as kyphosis or a “dowager’s hump.” This forward stoop can lead to balance issues, increasing the risk of falls and further fractures.
Respiratory and Digestive Issues
Severe spinal deformities from compression fractures can reduce lung capacity and make breathing more difficult. The change in posture can also compress abdominal organs, leading to digestive issues like acid reflux and reduced appetite.
Emotional and Psychological Impact
Living with chronic pain, limited mobility, and the fear of fractures can take an emotional toll. Individuals with osteoporosis may experience anxiety, depression, or social isolation due to decreased independence and lifestyle changes.
Increased Mortality Risk
Serious fractures, particularly hip fractures, are associated with an increased risk of mortality, especially in older adults. Complications like blood clots, infections, and reduced mobility following a fracture contribute to this risk.
Conclusion
Osteoporosis is often called the “silent disease” for a reason – it can progress unnoticed until a sudden fracture brings it to light. However, with greater awareness, early detection, and proactive management, the risks and complications associated with osteoporosis can be significantly reduced. If you or a loved one are at risk of osteoporosis or experiencing symptoms, don’t wait until it’s too late. Early diagnosis and intervention are key to maintaining strong bones and a better quality of life. Schedule a bone health assessment at Graphic Era Hospital today and take the first step towards protecting your bones for the future.
Frequently Asked Questions (FAQs)
Can osteoporosis be cured?
What is the best way to prevent osteoporosis?
The best way to prevent osteoporosis is by maintaining strong bones through a balanced diet rich in calcium and vitamin D, engaging in regular weight-bearing and strength-training exercises, avoiding smoking and excessive alcohol, and getting regular bone density screenings, especially if you have risk factors.
At what age should I get a bone density test?
What foods are best for bone health?
Foods rich in calcium and vitamin D are essential for bone health. Good sources of calcium include dairy products, leafy green vegetables, almonds, and fortified foods. Vitamin D can be found in fatty fish, fortified foods, and through adequate sun exposure. Foods rich in magnesium and vitamin K also support bone strength.
Can men develop osteoporosis?
Yes, while osteoporosis is more common in women, especially postmenopausal women, men can also develop the condition. Men over the age of 70 or those with risk factors such as low testosterone, certain medications, or chronic diseases are at an increased risk of osteoporosis.
By Specialities
- Bariatric Surgery
- Cancer Care
- Cardiology
- Dental
- Dermatology
- Diabetes & Endocrinology
- Endocrinology and Diabetes
- ENT (Ear Nose Throat)
- Eye Care
- Gastroenterology
- Haematology
- Health Awareness
- Health Care
- Health Tips
- Hematology
- Hepatology
- Internal Medicine
- Mental Health and Behavioural Sciences
- Metabolic
- Neonatology
- Nephrology
- Neurology
- Nutrition & Dietetics
- Obstetrics & Gynaecology
- Oncology
- Ophthalmology
- Orthopaedics
- Paediatric
- Physiotherapy & Rehabilitation
- Plastic and Reconstructive Surgery
- Psychology
- Pulmonology
- Rheumatology
- Spine
- Urology
Recent Posts
- World Hearing Day 2026: Empower Yourself to Protect and Improve Your Hearing
- Understanding Chickenpox: Early Signs, Treatment Options, and Recovery Tips
- Gallbladder and Bile Duct Cancer Awareness Month 2026: All You Need to Know
- High-Fibre Diet: Health Benefits and Top Fibre-Rich Foods
- Why Do My Gums Bleed While Brushing?
Need expert medical advice?
Share your details and our healthcare specialists will reach out to assist you.
By proceeding, you acknowledge and agree to our Privacy Policy, Terms of Use, and Disclaimer.