World Tuberculosis Day 2025: Symptoms, Treatment, and Prevention
Despite advancements in medical science, TB continues to pose a serious public health challenge, especially in low- and middle-income countries. To raise awareness and accelerate efforts to eliminate TB, World Tuberculosis Day is observed annually on 24th March. This global initiative highlights the importance of TB prevention, early diagnosis, and effective treatment in reducing its impact. In this article, we will discuss TB symptoms, risk factors, diagnosis, prevention, and treatment while highlighting the significance of World Tuberculosis Day 2025 in raising global awareness. But first, let’s understand the disease.
Table of Contents
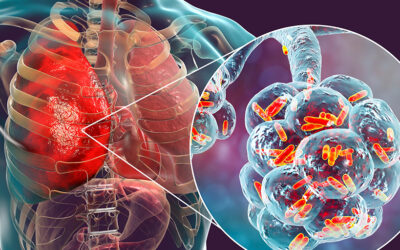
ToggleUnderstanding Tuberculosis: Causes and Transmission
Tuberculosis is an infectious disease caused by the bacterium Mycobacterium tuberculosis, primarily affecting the lungs (pulmonary tuberculosis). That said, it can also impact other parts of the body, such as the brain, spine, and kidneys. The disease spreads when an infected person coughs, sneezes, or speaks, releasing airborne droplets that can be inhaled by others.
How is TB Transmitted?
-
-
- Airborne transmission: TB bacteria spread through the air when a person with active tuberculosis expels bacteria-containing droplets.
- Close and prolonged contact: Individuals living or working in crowded environments are at higher risk of exposure.
- Latent vs. Active TB:
- Latent TB infection: The bacteria remain in the body without causing symptoms or spreading.
- Active TB disease: The infection becomes symptomatic and contagious, requiring immediate treatment.
-
TB transmission is not caused by sharing food, water, or physical contact, but untreated TB patients can unknowingly infect others. Early diagnosis and treatment are essential to controlling its spread.
Read more- Human Metapneumovirus (HMPV): Symptoms, Causes, Treatment & Risk Factors
What are the Symptoms of Tuberculosis?
Tuberculosis symptoms vary depending on whether the infection is pulmonary (affecting the lungs) or extrapulmonary (affecting other organs). While latent TB infection remains asymptomatic, active TB disease presents with noticeable signs that require immediate medical attention.
1. Common Symptoms of Pulmonary Tuberculosis
Pulmonary TB is the most common form of tuberculosis and primarily affects the lungs. Its symptoms include:
-
-
- Persistent cough lasting more than three weeks, often with mucus or blood.
- Unexplained weight loss due to loss of appetite.
- Fever and night sweats, common in active TB cases.
- Chest pain and difficulty breathing, caused by lung inflammation.
- Extreme fatigue and weakness, affecting daily activities.
-
2. Symptoms of Extrapulmonary Tuberculosis
When TB spreads beyond the lungs, it can affect various organs, leading to:
-
-
- Tuberculosis of the spine: Back pain and stiffness.
- TB meningitis (brain infection): Severe headache, confusion, and sensitivity to light.
- Lymph node TB: Swollen lymph nodes, especially in the neck.
- Abdominal TB: Pain, swelling, and digestive issues.
-
When to Seek Medical Attention
Early detection is crucial to prevent TB complications and transmission. Medical attention is necessary if:
-
-
- A persistent cough with blood or mucus lasts over three weeks.
- There is unexplained weight loss, fever, or night sweats.
- A person has been in close contact with a TB patient.
-
Recognising these warning signs and seeking timely TB diagnosis and treatment can prevent further spread and improve recovery outcomes.
Read more-Pulmonary Oedema: All You Need to Know
How is Tuberculosis Diagnosed?
Early and accurate diagnosis of tuberculosis is essential to prevent disease progression and transmission. TB can be latent (inactive) or active, and different diagnostic tests help detect the infection based on its stage.
1. Common Tests for Tuberculosis Diagnosis
Healthcare professionals use various methods to detect TB bacteria in the body:
-
-
- Tuberculin Skin Test (TST) or Mantoux Test:
- A small amount of tuberculin solution is injected under the skin.
- If a raised lump develops within 48-72 hours, it indicates exposure to TB bacteria.
- Cannot differentiate between latent TB infection and active TB disease.
- Interferon-Gamma Release Assays (IGRAs):
- A blood test that detects TB infection.
- Often used to confirm latent TB infection, especially in high-risk individuals.
- Chest X-ray and CT Scan:
- Used to identify lung abnormalities and detect pulmonary tuberculosis.
- Helps determine if TB is active but does not confirm the presence of bacteria.
- Sputum Tests (Microscopy and Culture):
- Sputum sample analysis detects TB bacteria in respiratory secretions.
- GeneXpert Test (PCR-based test) rapidly confirms TB and detects drug-resistant TB (MDR-TB).
- Culture test remains the gold standard but takes several weeks to produce results.
- Tuberculin Skin Test (TST) or Mantoux Test:
-
Early TB detection ensures timely treatment, reduces transmission risks, and prevents severe complications of tuberculosis. People with persistent symptoms, close TB contacts, or weakened immunity should get tested immediately.
Read more- Bronchiolitis: A Complete Guide for Parents
Tuberculosis Treatment
Tuberculosis is curable with proper medication and adherence to treatment protocols. TB treatment involves a combination of antibiotics taken over an extended period to eliminate the bacteria and prevent drug resistance.
Standard TB Treatment: The Six-Month Antibiotic Regimen
The primary treatment for drug-sensitive tuberculosis includes a six-month course of four key antibiotics:
-
-
- Rifampicin (RIF) – Destroys TB bacteria.
- Isoniazid (INH) – Prevents bacterial growth.
- Pyrazinamide (PZA) – Targets bacteria in inactive states.
- Ethambutol (EMB) – Prevents bacterial resistance.
-
Treatment Phases:
-
-
- Intensive Phase (First 2 months): All four antibiotics are taken daily to reduce bacterial load.
- Continuation Phase (Next 4 months): Two drugs (Rifampicin and Isoniazid) are continued to prevent relapse.
-
Missing doses or stopping treatment early can lead to drug-resistant TB, making future treatment more challenging.
Multidrug-Resistant TB (MDR-TB) and Its Treatment
MDR-TB occurs when the bacteria become resistant to Rifampicin and Isoniazid, the two most effective TB drugs. Treatment includes:
-
-
- Second-line antibiotics such as fluoroquinolones, aminoglycosides, and bedaquiline.
- A longer treatment duration (12-24 months) with increased side effects.
- Strict adherence to medication to improve cure rates and prevent further resistance.
-
Importance of Completing TB Treatment
-
-
- Skipping doses or stopping early can lead to relapse or drug resistance.
- Patients must follow the full treatment course, even if symptoms improve.
- Directly Observed Treatment, Short-course (DOTS) is used globally to ensure patients complete their TB regimen under supervision.
-
Timely TB treatment prevents complications, reduces TB transmission, and improves overall recovery.
Risk Factors for Tuberculosis
While anyone can get tuberculosis, certain factors increase the risk of infection, disease progression, and complications. Understanding these risk factors is essential for TB prevention and early intervention.
1. Weakened Immune System
A strong immune system helps the body fight Mycobacterium tuberculosis. However, individuals with compromised immunity are at higher risk of developing active TB. These include:
-
-
- HIV/AIDS patients: TB is a leading cause of death among people with HIV.
- People undergoing chemotherapy or organ transplants.
- Individuals with chronic illnesses such as diabetes, kidney disease, or cancer.
-
2. Malnutrition and Poor Living Conditions
Lack of proper nutrition weakens immunity, making it easier for latent TB infection to become active TB disease. People living in poverty-stricken areas with limited healthcare access, overcrowding, and poor ventilation are at greater risk of TB exposure.
3. Close Contact with TB-Infected Individuals
Those in regular contact with active TB patients, such as:
-
-
- Family members or caregivers of TB patients.
- Healthcare workers treating infected individuals.
- Residents of prisons, refugee camps, or shelters with poor ventilation.
-
4. Smoking and Substance Abuse
-
-
- Tobacco smokers are twice as likely to develop active TB due to lung damage.
- Excessive alcohol consumption and drug use weaken the immune system, increasing susceptibility.
-
5. Travel or Residence in High TB Burden Areas
People who live in or travel to TB-endemic regions, such as parts of Asia, Africa, and Eastern Europe, have a higher risk of exposure.
By addressing these risk factors, individuals and healthcare systems can work towards better tuberculosis prevention and early intervention strategies.
How to Reduce the Risk of Tuberculosis
Preventing tuberculosis requires vaccination, early detection, and effective public health strategies. By taking the right precautions, individuals and communities can reduce the risk of TB transmission and infection.
1. BCG Vaccine: Protection Against Severe TB
-
-
- The Bacillus Calmette-Guérin (BCG) vaccine is administered to infants in many countries to prevent severe forms of tuberculosis, such as TB meningitis and military TB.
- While it does not completely prevent pulmonary TB, it offers partial immunity against severe infections.
-
2. Personal Preventive Measures
Individuals can lower their TB risk by:
-
-
- Wearing masks and maintaining ventilation in crowded or high-risk environments.
- Practicing good hygiene, such as covering the mouth when coughing or sneezing.
- Avoiding close contact with active TB patients if not undergoing treatment.
- Ensuring proper nutrition, as malnutrition weakens immunity and increases susceptibility.
-
3. Public Health Strategies for TB Prevention
-
-
- Early screening and testing in high-risk populations.
- Contact tracing to identify and treat people exposed to TB patients.
- DOTS (Directly Observed Treatment, Short-course) to ensure patient adherence and reduce drug resistance.
-
By combining personal hygiene, vaccination, and public health interventions, TB cases can be significantly reduced, moving toward global tuberculosis eradication goals.
World Tuberculosis Day 2025: Global Efforts for Raising Awareness
World Tuberculosis Day, observed on 24th March, aims to spread awareness, eliminate stigma, and accelerate global efforts to end TB. It marks the discovery of the Mycobacterium tuberculosis bacterium by Dr. Robert Koch in 1882, a breakthrough in diagnosing and treating the disease.
How World TB Day Promotes Tuberculosis Awareness
-
-
- Educating the public on TB symptoms, transmission, and prevention.
- Encouraging early diagnosis and treatment adherence to reduce TB cases.
- Addressing misconceptions and stigma surrounding tuberculosis.
-
WHO and Global Initiatives to End TB
-
-
- End TB Strategy (WHO): Aims to reduce TB deaths by 90% by 2030.
- United Nations Sustainable Development Goals (SDGs): Focuses on eradicating TB as a major public health crisis.
- Governments and NGOs work to expand TB screening, vaccination, and treatment accessibility.
-
The Importance of Public Participation
-
-
- Individuals can join awareness campaigns and educate their communities.
- Governments and healthcare providers must prioritise TB control measures.
- Supporting research for better TB vaccines and treatments can aid eradication efforts.
-
By strengthening global and local initiatives, World Tuberculosis Day continues to drive efforts toward a TB-free world.
A Collective Effort to End Tuberculosis
Tuberculosis remains a global health challenge, but with early diagnosis, effective treatment, and preventive measures, it is both curable and preventable. World Tuberculosis Day 2025 serves as a reminder that raising TB awareness, improving access to healthcare, and supporting global initiatives are key to controlling the disease. If you or a loved one experience persistent cough, fever, weight loss, or other TB symptoms, seeking early medical intervention is crucial. Graphic Era Hospital offers expert TB diagnosis, advanced treatment, and preventive care to ensure the best outcomes for patients. Book a consultation today and take a step toward a healthier future.
Frequently Asked Questions About Tuberculosis (TB)
Is tuberculosis curable?
Who should get the BCG vaccine for TB prevention?
The BCG vaccine is recommended for infants in high-risk countries to prevent severe TB forms, such as TB meningitis. It does not fully prevent pulmonary TB but offers partial protection against severe complications.
What are the complications of untreated tuberculosis?
Can tuberculosis return after treatment?
Yes, TB can relapse if treatment is not completed properly or if the patient is re-exposed to the bacteria. Those with weakened immune systems (such as HIV patients) are at higher risk of reinfection or reactivation of latent TB.
By Specialities
- Bariatric Surgery
- Cancer Care
- Cardiology
- Dental
- Dermatology
- Diabetes & Endocrinology
- Endocrinology and Diabetes
- ENT (Ear Nose Throat)
- Eye Care
- Gastroenterology
- Haematology
- Health Awareness
- Health Care
- Health Tips
- Hematology
- Hepatology
- Internal Medicine
- Mental Health and Behavioural Sciences
- Metabolic
- Neonatology
- Nephrology
- Neurology
- Nutrition & Dietetics
- Obstetrics & Gynaecology
- Oncology
- Ophthalmology
- Orthopaedics
- Paediatric
- Physiotherapy & Rehabilitation
- Plastic and Reconstructive Surgery
- Psychology
- Pulmonology
- Rheumatology
- Spine
- Urology
Recent Posts
Need expert medical advice?
Share your details and our healthcare specialists will reach out to assist you.
By proceeding, you acknowledge and agree to our Privacy Policy, Terms of Use, and Disclaimer.