Acute and Chronic Bronchitis: Know the Difference and When to Seek Help

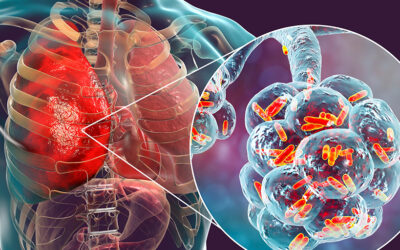
Breathing difficulty, cough, and chest congestion are common signs of bronchitis, a condition caused by inflammation of the bronchial tubes. Although the term bronchitis is used broadly, it includes two distinct forms: Acute bronchitis usually develops suddenly due to seasonal infections, while chronic bronchitis involves long-term airway irritation that gradually affects lung function. Understanding the difference between the two helps individuals recognise what their symptoms may suggest and seek timely assessment to protect long-term respiratory health. In this article, we explain the difference between acute and chronic bronchitis, their causes, diagnosis, treatment options, and the symptoms that require medical attention.
Table of Contents
ToggleUnderstanding Bronchitis
Bronchitis occurs when the bronchial tubes, which carry air in and out of the lungs, become inflamed. This inflammation causes the lining of these airways to swell and produce excess mucus, making it harder for air to pass freely. As the body attempts to clear the mucus, a cough develops, often accompanied by chest discomfort, breathlessness, or a feeling of tightness in the chest.
The condition can arise from infections or long-term irritation, and its impact varies depending on how long the inflammation lasts and what triggered it. Some episodes come on suddenly and improve within a short period, while others persist for months and gradually interfere with normal breathing.
Causes and Risk Factors of Acute and Chronic Bronchitis
Bronchitis develops when the airways become inflamed due to infections or long-term irritation. The underlying triggers and contributing factors differ between acute and chronic forms, which explains why some episodes resolve quickly while others persist or recur.
Acute Bronchitis: Causes and Risk Factors
Acute bronchitis usually appears suddenly and often follows an infection of the upper respiratory tract. Several causes and risk factors contribute to short-term airway inflammation, such as:
- Viral infections: Seasonal viruses such as influenza, rhinovirus, and respiratory syncytial virus commonly trigger airway inflammation.
- Bacterial infections: Certain bacteria may cause acute bronchitis, especially when a viral illness has already weakened the respiratory system.
- Sudden exposure to irritants: Smoke, chemical vapours, or polluted air can inflame the bronchial tubes and cause temporary symptoms.
- Seasonal viral outbreaks: Higher infection rates during winter and monsoon seasons increase the likelihood of acute episodes.
- Lowered immunity: Illness, stress, or poor nutrition can increase susceptibility to infections.
- Close contact with infected individuals: Crowded settings, workplaces, and schools raise exposure risk.
- History of frequent respiratory infections: Repeated colds or flu can make the airways more sensitive.
Chronic Bronchitis: Causes and Risk Factors
Chronic bronchitis develops when the airways experience repeated irritation over an extended period. This long-term inflammation is influenced by several causes and contributing factors, including:
- Long-term cigarette smoking: Tobacco smoke is the leading cause and continuously irritates and damages the airway lining.
- Occupational exposure: Jobs involving dust, chemicals, industrial fumes, or strong odours increase the risk of chronic airway damage.
- Air pollution: Prolonged exposure to polluted indoor or outdoor air, especially particulate matter such as PM2.5 and PM10, can irritate the bronchi and contribute to chronic inflammation.
- Indoor pollutants: Biomass fuel, poorly ventilated kitchens, or frequent exposure to indoor smoke may gradually harm the airways.
- Existing lung conditions: Asthma and recurrent respiratory problems raise susceptibility to chronic airway irritation.
Symptoms of Acute and Chronic Bronchitis
Bronchitis affects the airways in different ways depending on whether the condition is short-term or long-standing. The symptoms often provide important clues that help distinguish between acute and chronic forms.
Symptoms of Acute Bronchitis
Acute bronchitis symptoms appear suddenly and usually improve within a few days or weeks. Common symptoms include:
- Persistent cough: Often begins dry and later produces mucus.
- Chest discomfort: A heavy or tight feeling in the chest.
- Mild fever or chills: Usually low-grade and linked to viral infections.
- Shortness of breath: Breathing may feel slightly more difficult during activity.
- Fatigue: The body uses extra energy to fight the infection, causing tiredness.
Chronic Bronchitis Symptoms
Chronic bronchitis involves continuous airway inflammation, and symptoms tend to be more persistent and noticeable over months. These may include:
- Daily productive cough: Lasts for at least three months a year for two consecutive years.
- Thick mucus production: Often increases during flare-ups.
- Breathlessness: Especially during routine activities due to reduced airflow.
- Frequent respiratory infections: Episodes may trigger worsening symptoms.
- Wheezing or noisy breathing: Caused by narrowed or irritated airways.
These symptoms show how acute bronchitis tends to resolve quickly, while chronic bronchitis progresses more gradually and often requires long-term management.
Key Differences Between Acute and Chronic Bronchitis
Although both conditions involve inflammation of the bronchial tubes, several features set them apart. Understanding these differences helps in recognising the pattern, severity, and long-term impact of each form. Key difference include:
| Parameter | Acute Bronchitis | Chronic Bronchitis |
| Duration | Short-term condition that lasts from a few days to a few weeks | Long-standing condition with symptoms that persist for months and recur over consecutive years |
| Primary Cause | Viral or bacterial infections affecting the respiratory tract | Long-term airway irritation due to smoking, pollution, or occupational exposure |
| Onset | Sudden onset after an infection or exposure to irritants | Gradual onset caused by continuous airway irritation |
| Symptom Pattern | Temporary cough, mild fever, chest discomfort, and mucus build-up | Daily productive cough, breathlessness, thick mucus, and frequent flare-ups |
| Progression | Resolves with rest and supportive care without long-term airway damage | Causes persistent inflammation and reduced lung function, often associated with COPD |
| Recurrence | Occasional and usually seasonal | Frequent episodes throughout the year |
| Complications | Rare, but may lead to pneumonia in high-risk individuals | Higher risk of respiratory failure, COPD progression, and repeated infections |
When to See a Doctor?
Bronchitis symptoms often improve with time, but certain warning signs indicate that the condition needs prompt medical attention. These red flags help identify when the inflammation is more severe, persistent, or affecting overall lung function. Individuals should seek medical care if they experience:
- Breathing difficulty that worsens or affects routine activities.
- A cough that persists longer than expected, especially if it continues beyond three weeks.
- High or prolonged fever, which may signal a secondary infection.
- Chest pain or tightness that disrupts sleep or daily comfort.
- Blood in the mucus, even in small amounts.
- Repeated episodes of bronchitis, which may indicate chronic airway irritation.
- Severe fatigue or inability to carry out normal tasks due to breathing issues.
- Worsening symptoms in individuals with asthma, COPD, or heart conditions, as flare-ups can escalate quickly.
Diagnosis of Acute and Chronic Bronchitis
Accurate diagnosis helps determine whether bronchitis is a short-term infection or part of a long-standing respiratory condition. Doctors assess symptoms, examine the lungs, and use specific tests to understand how the airways are functioning. The diagnostic approach include:
Clinical Evaluation
Doctors begin with a detailed evaluation, which includes:
- Medical history review: Understanding symptom duration, frequency, and exposure to infections or irritants.
- Physical examination: Listening to the lungs for wheezing, crackles, or reduced airflow.
Tests and Imaging
Further tests help confirm the diagnosis and assess the severity of airway inflammation:
- Chest X-ray: Helps rule out pneumonia or other lung problems.
- Pulmonary function tests: Measure how well the lungs move air in and out, especially useful for chronic bronchitis.
- Sputum analysis: Identifies infection-causing organisms when symptoms are severe or prolonged.
- Oxygen saturation check: Assesses oxygen levels in the blood during breathing difficulties.
Identifying Chronic Patterns
Doctors diagnose chronic bronchitis when symptoms such as a productive cough persist for at least three months a year for two consecutive years. Assessments help determine whether the condition forms part of chronic obstructive pulmonary disease and guide long-term management.
Treatment Options for Acute and Chronic Bronchitis
Treatment aims to reduce airway inflammation, ease breathing, and prevent complications. The approach differs depending on whether the condition is temporary or long-standing.
Acute Bronchitis Treatment
Doctors focus on relieving symptoms while the body recovers from the infection. Treatment commonly includes:
- Rest and hydration: Help the airway lining heal and loosen mucus.
- Pain relievers or fever medication: Reduce discomfort caused by inflammation.
- Cough remedies: Support better sleep and reduce irritation; used only when medically appropriate.
- Short-term inhalers: Ease breathing in individuals with wheezing or tightness.
- Antibiotics only when needed: Reserved for confirmed or suspected bacterial infections.
Chronic Bronchitis Treatment
Long-term inflammation requires structured management to improve airflow and prevent flare-ups. Treatment may include:
- Bronchodilators: Relax the airway muscles and improve breathing.
- Inhaled corticosteroids: Reduce chronic inflammation and ease symptoms.
- Pulmonary rehabilitation: Involves breathing exercises and supervised activity to strengthen lung function.
- Long-term oxygen therapy: Recommended in severe cases with low oxygen levels.
- Vaccinations: Annual flu shots and pneumonia vaccines lower the risk of infections that worsen symptoms.
Managing Flare-Ups
Individuals with chronic bronchitis may experience episodes that resemble acute bronchitis. During flare-ups, doctors may adjust inhalers, prescribe short courses of steroids, or recommend stronger medications to control sudden inflammation.
These treatments aim to restore comfort, protect lung health, and reduce the chances of repeated respiratory episodes.
Recovery and Outlook
Recovery from bronchitis depends on the type of inflammation, overall lung health, and the presence of any underlying conditions. Acute bronchitis resolves relatively quickly, while chronic bronchitis requires ongoing management to maintain stable breathing.
Acute Bronchitis Recovery
Most people recover from acute bronchitis within a few days to a few weeks as the infection clears. Rest, hydration, and supportive care help the airway lining heal. A lingering cough may continue for a short period even after other symptoms improve because the airways take time to fully settle. With timely care, the long-term outlook is generally good.
Chronic Bronchitis Recovery Time
Chronic bronchitis progresses more gradually and requires consistent treatment to keep symptoms under control. Recovery focuses on improving airflow, reducing flare-ups, and slowing the progression of airway damage. Factors such as smoking cessation, regular medication use, and avoiding pollutants play an important role in long-term stability. Although chronic bronchitis cannot be reversed completely, structured care helps individuals maintain a better quality of life.
Complications Associated with Bronchitis
Complications vary depending on whether the inflammation is short-term or long-standing. Understanding these risks helps highlight why timely care and ongoing monitoring are important for lung health.
Complications of Acute Bronchitis
Acute bronchitis usually resolves without long-term problems, but certain complications may occur in vulnerable individuals. These include:
- Pneumonia: The infection may spread deeper into the lungs, especially in older adults or those with weak immunity.
- Persistent cough: Some people experience a prolonged cough as the airways take time to heal.
- Worsening of underlying conditions: Asthma, COPD, or heart problems may flare up during an acute episode.
Complications of Chronic Bronchitis
Chronic bronchitis carries a higher risk of long-term respiratory problems due to repeated airway inflammation. Possible complications include:
- Chronic obstructive pulmonary disease progression: Ongoing inflammation gradually reduces lung function.
- Frequent respiratory infections: Damaged airways are more prone to recurrent infections and hospital visits.
- Respiratory failure: In advanced cases, the lungs may struggle to maintain adequate oxygen levels.
- Reduced exercise tolerance: Breathlessness and low oxygen levels may limit routine activities over time.
These complications show why early assessment, preventive care, and long-term monitoring play a crucial role in protecting respiratory health.
Prevention of Acute and Chronic Bronchitis
Preventive measures play an important role in reducing the frequency, severity, and impact of bronchitis. The strategies differ for acute and chronic forms because each has unique triggers.
Prevention of Acute Bronchitis
Simple habits and seasonal precautions can lower the risk of short-term airway inflammation:
- Hand hygiene: Regular handwashing reduces exposure to viruses that commonly cause acute bronchitis.
- Avoiding close contact during outbreaks: Staying cautious in crowded or poorly ventilated areas helps prevent infections.
- Using masks during seasonal infections: Particularly useful during flu season or high viral circulation.
- Staying up to date with vaccinations: Flu and pneumonia vaccines help prevent infections that may trigger bronchitis.
- Strengthening immunity: Adequate sleep, balanced nutrition, and stress control support better respiratory health.
Prevention of Chronic Bronchitis
Long-term airway health depends on reducing exposure to irritants and protecting the lungs from ongoing damage. Key measures include:
- Stopping smoking: The most effective step to prevent chronic bronchitis and slow disease progression.
- Limiting exposure to pollutants: Using masks in polluted environments and ensuring good indoor ventilation.
- Workplace protection: Wearing safety gear in jobs involving dust, fumes, or chemical vapours.
- Regular lung check-ups: Early assessment helps detect airway changes before symptoms worsen.
- Managing underlying conditions: Proper control of asthma or respiratory allergies lowers the chance of chronic airway irritation.
These preventive steps support healthier airways, reduce the risk of recurrent episodes, and improve long-term respiratory well-being.
Why Choose Graphic Era Hospital for Bronchitis Care?
Effective management of bronchitis requires accurate diagnosis, expert guidance, and a care plan tailored to the severity and type of airway inflammation. At Graphic Era Hospital, the focus remains on providing safe, reliable, and patient-centred respiratory care through every stage of evaluation and treatment. Here’s why people choose Graphic Era Hospital for bronchitis care:
Experienced Pulmonary Specialists
At Graphic Era Hospital, our team of pulmonologists have extensive experience in evaluating both acute and chronic bronchitis. They review symptoms in detail, identify the specific factors causing airway inflammation, and create evidence-based treatment plans that focus on relieving discomfort, improving airflow, and protecting long-term lung health.
Advanced Technology and Imaging
We, at Graphic Era Hospital, use high-quality diagnostic tools such as chest X-rays, pulmonary function tests, and oxygen monitoring systems to evaluate airway inflammation with precision. These technologies help doctors understand the extent of irritation and plan treatment effectively.
Comprehensive Rehabilitation and Personalised Care
Patients receive individualised guidance based on their symptoms, lung function, and risk factors. Breathing exercises, inhaler techniques, lifestyle recommendations, and preventive strategies are explained clearly to ensure meaningful improvement and better day-to-day comfort.
Dietary and Lifestyle Recommendations for Better Lung Health
Supportive lifestyle habits play an important role in easing airway irritation, strengthening lung function, and reducing the frequency of respiratory flare-ups. These changes complement medical treatment and help maintain long-term respiratory well-being.
Dietary Recommendations
Balanced nutrition helps the body recover from inflammation and maintain stronger immunity. The following dietary choices support better lung health:
- Foods rich in dietary fibre: Whole grains, dals, millets, and vegetables support overall wellness and help reduce inflammation.
- Antioxidant-rich fruits: Indian options such as amla, oranges, guava, papaya, and pomegranate help protect lung tissue.
- Warm fluids: Soups, herbal teas, and warm water help loosen mucus and improve comfort.
- Healthy fats: Nuts, seeds, and small amounts of cold-pressed oils support better respiratory function.
- Adequate hydration: Water helps thin mucus and improves airway clearance.
Lifestyle Recommendations
Daily habits influence how well the airways cope with irritants. The following practices support healthier breathing:
- Maintaining clean indoor air: Using exhaust fans, keeping rooms ventilated, and reducing incense or smoke exposure.
- Breathing exercises: Simple techniques such as pursed-lip breathing and deep breathing improve airflow and lung capacity.
- Regular physical activity: Light walking or stretching helps maintain stamina without overexertion.
- Avoiding smoke and fumes: Staying away from cigarette smoke, industrial fumes, and polluted environments whenever possible.
- Monitoring seasonal changes: Wearing masks during high pollution periods or viral outbreaks helps reduce irritation.
Conclusion
Recognising the difference between acute and chronic bronchitis helps in understanding how the condition behaves, what triggers it, and when medical care becomes necessary. Early assessment, timely treatment, and supportive lifestyle habits play a vital role in maintaining respiratory comfort and overall well-being.
For individuals experiencing persistent or worsening breathing issues, expert evaluation can guide the next steps and help prevent complications. To book a consultation with a pulmonologist at Graphic Era Hospital, call 1800-889-7351.
Frequently Asked Questions (FAQs)
What is the main difference between acute and chronic bronchitis?
Acute bronchitis develops suddenly due to an infection and usually improves within a few weeks. Chronic bronchitis involves long-term airway irritation that causes a persistent cough and mucus production for months.
How long does chronic bronchitis recovery usually take?
Chronic bronchitis does not resolve completely, but symptoms improve with long-term management, inhaled medications, and avoidance of irritants such as smoke and pollution.
Does acute bronchitis always need antibiotics?
No. Most acute bronchitis cases result from viral infections, so antibiotics are not required unless a doctor suspects a bacterial cause.
When should someone visit a pulmonologist for bronchitis symptoms?
A visit is necessary if symptoms last more than three weeks, breathing becomes difficult, or episodes occur repeatedly. Individuals in Dehradun searching for a “bronchitis doctor near me” can seek timely evaluation from a respiratory specialist.
Is bronchitis contagious?
Only acute bronchitis caused by viral or bacterial infections can spread from person to person. Chronic bronchitis is not contagious.
How can air pollution affect chronic bronchitis?
Long-term exposure to polluted air can worsen airway inflammation, increase mucus production, and trigger flare-ups in individuals with chronic bronchitis.
Can chronic bronchitis turn into COPD?
Yes. Chronic bronchitis is considered a form of chronic obstructive pulmonary disease, and long-standing inflammation can gradually reduce lung function over time.
By Specialities
- Bariatric Surgery
- Cancer Care
- Cardiology
- Dental
- Dermatology
- Diabetes & Endocrinology
- Endocrinology and Diabetes
- ENT (Ear Nose Throat)
- Eye Care
- Gastroenterology
- Haematology
- Health Awareness
- Health Care
- Health Tips
- Hematology
- Hepatology
- Internal Medicine
- Mental Health and Behavioural Sciences
- Metabolic
- Neonatology
- Nephrology
- Neurology
- Nutrition & Dietetics
- Obstetrics & Gynaecology
- Oncology
- Ophthalmology
- Orthopaedics
- Paediatric
- Physiotherapy & Rehabilitation
- Plastic and Reconstructive Surgery
- Psychology
- Pulmonology
- Rheumatology
- Spine
- Urology
Recent Posts
- Bacterial and Viral Pneumonia: Causes, Symptoms, and Treatment Options
- World Hearing Day 2026: Empower Yourself to Protect and Improve Your Hearing
- Understanding Chickenpox: Early Signs, Treatment Options, and Recovery Tips
- Gallbladder and Bile Duct Cancer Awareness Month 2026: All You Need to Know
- High-Fibre Diet: Health Benefits and Top Fibre-Rich Foods
Need expert medical advice?
Share your details and our healthcare specialists will reach out to assist you.
By proceeding, you acknowledge and agree to our Privacy Policy, Terms of Use, and Disclaimer.