Bacterial and Viral Pneumonia: Causes, Symptoms, and Treatment Options
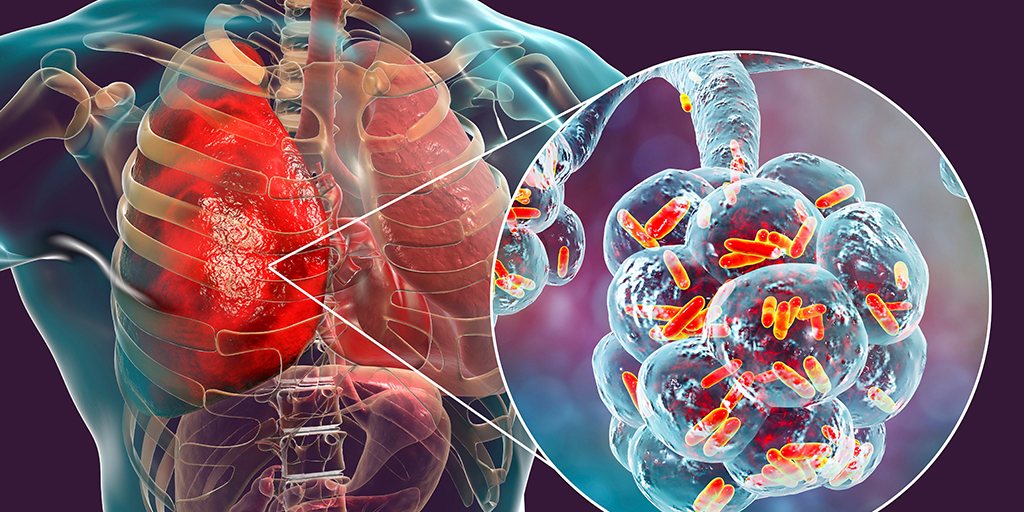
Pneumonia is a lung infection that causes inflammation of the air sacs (alveoli), making breathing difficult and reducing the amount of oxygen that reaches the bloodstream. It can affect people of all ages, but young children, older adults, and individuals with weakened immunity are at a higher risk of developing severe illness.
Among the different types of pneumonia, bacterial and viral pneumonia are the most common and account for the majority of cases seen in clinical practice. Although both conditions affect the lungs, their causes, progression, and treatment approaches differ in important ways. Understanding these differences helps patients and families recognise symptoms early, seek timely medical care, and ensure appropriate treatment.
Table of Contents
ToggleUnderstanding Bacterial and Viral Pneumonia
Both bacterial and viral pneumonia involve infection of the lungs, but they differ in how the infection develops and affects lung tissue. In pneumonia, the air sacs that normally fill with air become inflamed and may fill with fluid or pus. This reduces the lungs’ ability to deliver oxygen to the body, leading to breathlessness and fatigue.
While bacterial pneumonia often causes a more intense inflammatory response, resulting in faster symptom onset and greater severity, viral pneumonia usually develops more gradually and may initially resemble a common respiratory infection. In some cases, viral pneumonia weakens the lungs, creating an opportunity for bacteria to cause a secondary infection, which can worsen symptoms significantly.
Causes of Viral Pneumonia
Viral pneumonia is caused by viruses that infect the respiratory tract and spread to the lungs. These infections are often transmitted through droplets released during coughing, sneezing, or close contact with an infected person.
Once inside the lungs, viruses trigger inflammation that narrows the airways and interferes with normal breathing. Viral pneumonia is more common during seasonal outbreaks of respiratory infections and tends to affect children and older adults more frequently.
People with weakened immune systems, chronic lung disease, heart disease, or those recovering from recent illnesses may find it harder to clear the virus, increasing the risk of complications.
Causes of Bacterial Pneumonia
Bacterial pneumonia occurs when bacteria enter the lungs and multiply, leading to infection. This can happen after inhaling infected droplets, aspirating bacteria from the mouth or throat, or as a complication following a viral respiratory infection.
Bacterial pneumonia often develops suddenly and can progress rapidly. Factors that increase susceptibility include smoking, alcohol use, diabetes, chronic lung conditions, prolonged bed rest, or recent hospitalisation. Older adults and individuals with compromised immunity are particularly vulnerable to severe bacterial infections of the lungs.
Symptoms of Bacterial and Viral Pneumonia
The symptoms of pneumonia can vary depending on the cause of infection, the age of the patient, and their overall health. While bacterial and viral pneumonia share several common features, the way symptoms develop and their severity often provide important clues about the underlying cause.
In many cases, symptoms begin mildly and worsen over time. In others, especially with bacterial infections, illness may develop suddenly and progress rapidly. Recognising these patterns can help patients and families seek medical care at the right time.
Common symptoms seen in both bacterial and viral pneumonia:
- Persistent cough
- Fever, with or without chills
- Shortness of breath, especially during physical activity
- Chest pain that worsens with coughing or deep breathing
- Fatigue, weakness, and reduced appetite
These symptoms reflect inflammation in the lungs and reduced oxygen exchange, which affects the body’s overall energy levels and breathing capacity.
Symptoms more commonly associated with bacterial pneumonia:
- Sudden onset of illness
- High fever, often accompanied by chills
- Cough producing thick, yellow or green mucus
- Sharp or stabbing chest pain
- Rapid breathing or an increased heart rate
Bacterial pneumonia often causes more intense inflammation, which explains the abrupt onset and more severe symptoms seen in many patients.
Symptoms more commonly associated with viral pneumonia:
- Gradual worsening of symptoms
- Dry cough in the early stages
- Headache and body aches
- Wheezing or a feeling of tightness in the chest
Viral pneumonia frequently begins like a common respiratory infection and may take several days to involve the lungs more significantly.
In older adults, symptoms can be less typical. Instead of fever or a strong cough, pneumonia may present as confusion, dizziness, worsening weakness, or a sudden decline in daily functioning. These subtle signs should never be ignored, as pneumonia in older individuals can progress quickly if left untreated.
How Pneumonia Is Diagnosed
Diagnosing pneumonia involves more than confirming the presence of a lung infection. Doctors must also determine how severe the infection is and whether it is more likely to be bacterial or viral, as this directly influences treatment decisions. Because symptoms alone are not always reliable indicators, diagnosis relies on a combination of clinical assessment and targeted investigations.
The process usually begins with a detailed medical history, including the duration and progression of symptoms, recent respiratory illnesses, exposure to infections, and any underlying health conditions. A physical examination follows, during which the doctor listens to the lungs for abnormal breath sounds such as crackles, wheezing, or areas where airflow appears reduced—signs that suggest inflammation or fluid in the lungs.
To confirm the diagnosis and assess the extent of lung involvement, doctors may recommend one or more diagnostic tests.
Diagnostic tests may include:
- Chest X-ray, which helps confirm pneumonia by showing areas of lung inflammation, consolidation, or fluid accumulation, and can also indicate how widespread the infection is
- Blood tests to detect signs of infection and inflammation, assess oxygen levels, and evaluate how the body is responding to the illness
- Sputum examination, particularly when bacterial pneumonia is suspected, to identify the organism responsible and guide the choice of antibiotics
- Tests for viral infections when clinical findings suggest a viral cause or when identifying the virus may influence treatment or infection control measures
- Pulse oximetry, a non-invasive test that measures oxygen saturation and helps determine whether oxygen support or hospital care is needed
The selection of tests depends on several factors, including symptom severity, patient age, existing medical conditions, and whether the infection is being managed at home or in hospital. In more severe cases, or when symptoms do not improve as expected, additional investigations may be required to identify complications or refine the diagnosis.
Treatment Options for Viral Pneumonia
Treatment of viral pneumonia focuses on supporting the body while it clears the infection. Because viruses are not affected by antibiotics, the primary goal of care is to relieve symptoms, maintain adequate oxygen levels, and prevent the infection from progressing to more severe illness.
For individuals with mild symptoms, treatment is usually provided at home. Rest is essential, as the body requires additional energy to fight the infection. Adequate fluid intake helps prevent dehydration and keeps respiratory secretions thinner, making coughing more effective and reducing discomfort.
Medications may be prescribed to control fever, body aches, and chest discomfort, which can significantly improve comfort and support recovery. In some cases, inhaled medications may be used to ease breathing, particularly if wheezing or chest tightness is present.
If viral pneumonia affects oxygen levels, oxygen therapy may be required to ensure that the body receives enough oxygen. This is more common in older adults, people with underlying lung or heart conditions, and those with more extensive lung involvement. Hospital care may be necessary for individuals who experience worsening breathlessness, persistent low oxygen levels, dehydration, or difficulty maintaining adequate nutrition.
Most people with viral pneumonia recover fully with appropriate supportive care. However, symptoms such as cough, tiredness, and reduced stamina may persist for several weeks, even after the infection has resolved. Gradual return to normal activities and follow-up care help ensure complete recovery and reduce the risk of complications.
Treatment Options for Bacterial Pneumonia
Treatment of bacterial pneumonia focuses on eliminating the infection while supporting lung function and preventing complications. Because bacterial infections can progress rapidly, timely medical treatment is essential to achieve good outcomes and reduce the risk of severe illness.
Antibiotics form the cornerstone of treatment for bacterial pneumonia. The choice of antibiotic depends on several factors, including the suspected or identified bacteria, the severity of symptoms, and the patient’s age and overall health. In mild cases, oral antibiotics may be sufficient and can be taken at home under medical supervision. It is important to complete the full course of antibiotics, even if symptoms begin to improve early, to ensure complete clearance of the infection.
In more severe cases, hospitalisation may be required. Intravenous antibiotics are often used when symptoms are intense, oxygen levels are low, or the patient has underlying health conditions that increase the risk of complications. Alongside antibiotics, supportive measures such as fever control, pain relief, and adequate hydration are provided to support recovery.
Oxygen therapy may be needed if lung inflammation significantly affects breathing or oxygen levels. Close monitoring allows doctors to assess response to treatment and adjust medications if necessary. In individuals who do not respond as expected, further investigations may be carried out to confirm the diagnosis or rule out complications.
With prompt and appropriate treatment, most people with bacterial pneumonia begin to improve within a few days. However, full recovery may take longer, and lingering fatigue or cough is not uncommon. Follow-up care helps ensure that the infection has resolved completely and that lung function returns to normal.
Possible Complications of Pneumonia
Complications of pneumonia are uncommon when the condition is diagnosed early and treated appropriately. However, they are more likely to occur in severe infections, delayed treatment, or in people with weakened immunity or existing medical conditions.
In such cases, pneumonia can place significant strain on the lungs and other organs, leading to complications that may require additional medical care.
Possible complications include:
- Fluid buildup around the lungs, which can interfere with normal breathing
- Lung abscess, where pockets of infection develop within lung tissue
- Respiratory failure, requiring oxygen support or assisted ventilation
- Spread of infection to the bloodstream, which can lead to a serious systemic illness
Prompt diagnosis, timely treatment, and proper follow-up significantly reduce the risk of these complications and improve overall outcomes.
Preventing Bacterial and Viral Pneumonia
Preventing pneumonia focuses on reducing exposure to infection, strengthening the body’s natural defences, and protecting individuals who are at higher risk of severe illness. While not all cases can be prevented, a combination of medical and lifestyle measures can significantly lower the risk of both viral and bacterial pneumonia.
One of the most effective preventive strategies is vaccination. Vaccines against influenza help reduce the risk of viral pneumonia and also lower the chance of secondary bacterial infections that can follow flu. Pneumococcal vaccines protect against common bacterial causes of pneumonia and are particularly important for older adults, young children, and people with chronic medical conditions.
In addition to building immunity through vaccination, limiting exposure to infectious organisms is equally important. Good respiratory hygiene—such as regular handwashing, covering the mouth and nose when coughing or sneezing, and avoiding close contact with people who have active respiratory infections, helps reduce the spread of viruses and bacteria that can lead to pneumonia.
Protecting lung health further reduces vulnerability to infection. Avoiding smoking is especially important, as smoking damages the lungs’ natural defence mechanisms and makes it easier for infections to take hold. Proper management of chronic conditions such as asthma, diabetes, and heart disease also strengthens the body’s ability to respond effectively to respiratory infections.
Finally, early recognition and treatment of respiratory illnesses play a key role in prevention. Seeking medical advice when symptoms such as persistent cough, fever, or breathlessness appear can prevent mild infections from progressing to pneumonia. Adequate rest, balanced nutrition, and good hydration support the immune system and aid recovery.
By addressing immunity, exposure, lung health, and early care together, the risk of bacterial and viral pneumonia can be significantly reduced, particularly among vulnerable individuals.
When to Seek Prompt Medical Attention
While mild cases of pneumonia may improve with appropriate treatment, certain symptoms require prompt medical evaluation. Seeking care early is especially important for older adults, young children, and individuals with underlying health conditions, as pneumonia can progress more rapidly in these groups.
Medical attention should be sought if symptoms such as high or persistent fever, worsening shortness of breath, chest pain, or a cough that does not improve develop. Increasing fatigue, confusion, dizziness, or difficulty performing routine activities may also indicate that the infection is affecting the body more seriously.
Urgent medical care is needed if breathing becomes laboured, oxygen levels appear low, lips or fingertips develop a bluish colour, or symptoms worsen despite treatment. Early evaluation allows doctors to assess the severity of the infection, adjust treatment if necessary, and prevent complications.
Consult a General Physician at Graphic Era Hospital
Experiencing persistent cough, breathlessness, fever, or chest discomfort? Our team of experienced general physicians at Graphic Era Hospital is here to help. The team carefully evaluates your symptoms, conducts the necessary investigations, and develops an appropriate care plan based on your condition and overall health.
Whether you require further assessment, treatment guidance, or close monitoring during recovery, we are committed to supporting you at every stage. Early medical attention can make a meaningful difference in recovery and help prevent complications.
Call 1800 889 7351 today to schedule a consultation and take the next step toward better respiratory health.
Frequently Asked Questions (FAQs)
Is pneumonia contagious?
Pneumonia itself is not directly contagious, but the viruses or bacteria that cause it can spread from person to person through respiratory droplets. Not everyone exposed will develop pneumonia, as individual immunity and overall health play an important role.
Can pneumonia return after recovery?
Yes, it is possible to develop pneumonia again, especially in individuals with weakened immunity, chronic lung conditions, or repeated respiratory infections. Preventive measures and follow-up care help reduce this risk.
How long should coughing last after pneumonia?
A lingering cough is common after pneumonia and may persist for several weeks as the lungs continue to heal. Gradual improvement is expected, but a cough that worsens or fails to improve should be medically evaluated.
Is pneumonia more dangerous in certain age groups?
Yes. Infants, older adults, and people with chronic medical conditions or weakened immune systems are at higher risk of severe illness and complications from pneumonia.
Can pneumonia affect lung function long term?
Most people recover fully without lasting lung damage. However, severe pneumonia or repeated infections may lead to prolonged weakness or reduced lung capacity, particularly in older adults or those with underlying lung disease.
Is hospitalisation always required for pneumonia?
No. Many cases of pneumonia can be treated at home under medical supervision. Hospital care is usually needed when symptoms are severe, oxygen levels are low, or the patient has risk factors that require close monitoring.
Can pneumonia be prevented completely?
While not all cases can be prevented, vaccinations, good respiratory hygiene, and early treatment of infections significantly lower the risk and severity of pneumonia.
When should follow-up be done after pneumonia treatment?
Follow-up is typically advised if symptoms persist, recovery feels slow, or complications are suspected. In some cases, doctors may recommend repeat evaluation to ensure the lungs have healed properly.
By Specialities
- Bariatric Surgery
- Cancer Care
- Cardiology
- Dental
- Dermatology
- Diabetes & Endocrinology
- Endocrinology and Diabetes
- ENT (Ear Nose Throat)
- Eye Care
- Gastroenterology
- Haematology
- Health Awareness
- Health Care
- Health Tips
- Hematology
- Hepatology
- Internal Medicine
- Mental Health and Behavioural Sciences
- Metabolic
- Neonatology
- Nephrology
- Neurology
- Nutrition & Dietetics
- Obstetrics & Gynaecology
- Oncology
- Ophthalmology
- Orthopaedics
- Paediatric
- Physiotherapy & Rehabilitation
- Plastic and Reconstructive Surgery
- Psychology
- Pulmonology
- Rheumatology
- Spine
- Urology
Recent Posts
- Bacterial and Viral Pneumonia: Causes, Symptoms, and Treatment Options
- World Hearing Day 2026: Empower Yourself to Protect and Improve Your Hearing
- Understanding Chickenpox: Early Signs, Treatment Options, and Recovery Tips
- Gallbladder and Bile Duct Cancer Awareness Month 2026: All You Need to Know
- High-Fibre Diet: Health Benefits and Top Fibre-Rich Foods
Need expert medical advice?
Share your details and our healthcare specialists will reach out to assist you.
By proceeding, you acknowledge and agree to our Privacy Policy, Terms of Use, and Disclaimer.