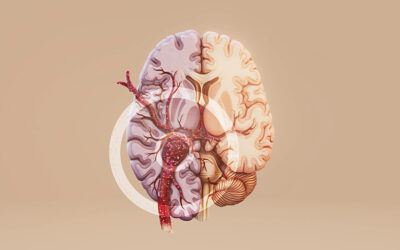
What is a Stroke: Causes, Symptoms & Treatment

A stroke occurs when blood flow to the brain is suddenly interrupted or there is bleeding in the brain, causing brain cells to die within minutes from lack of oxygen. This medical emergency affects someone every 40 seconds worldwide, making it one of the leading causes of death and disability globally. What makes stroke particularly critical is that it demands immediate action. The faster treatment begins, the better the chances of recovery and minimising long-term damage.
This comprehensive guide will cover what a stroke is, how to identify its warning signs, what immediate steps to take, and the treatment options available. But before we get into the details, let’s start by understanding what a stroke is.
Table of Contents
ToggleWhat is Ischemic Stroke?
A stroke occurs when the blood flow to a part of the brain is blocked or significantly reduced, preventing brain cells from receiving the oxygen and nutrients they need to function. Without an adequate blood supply, brain cells start to die within minutes, which can cause permanent brain damage if treatment is delayed. The effects of a stroke depend on which area of the brain is affected and how severe the damage is. In addition to physical and cognitive effects, a stroke can also impact vision, balance, and coordination, and in severe cases, it may be life-threatening.
Types of Strokes
There are two main types of stroke, each caused by different problems with blood flow to the brain, along with a less common type that is harder to pinpoint.
Ischemic Stroke
Ischemic stroke occurs when a blood vessel supplying the brain is blocked, usually by a blood clot or a buildup of fatty deposits called plaque. This blockage stops oxygen and nutrients from reaching the brain cells, causing them to die. It is the most common type of stroke, accounting for nearly 87% of all cases. Symptoms can appear suddenly and may include weakness or numbness on one side of the body, difficulty speaking or understanding speech, and vision problems.
Haemorrhagic Stroke
A haemorrhagic stroke happens when a blood vessel in the brain bursts, leading to bleeding inside or around the brain. The leaking blood increases pressure on the brain and damages brain tissue. High blood pressure is the most common cause, but aneurysms or head injuries can also trigger this type of stroke. Hemorrhagic strokes are less common than ischemic strokes but are often more severe and require urgent medical attention.
Cryptogenic Stroke
Cryptogenic stroke refers to a stroke with no clearly identifiable cause even after thorough medical evaluation. It accounts for a significant number of strokes and may result from hidden heart conditions, blood clotting disorders, or other undetected issues. Identifying risk factors and monitoring for underlying conditions is crucial for preventing recurrence.
What Causes Strokes?
Strokes occur when the brain does not receive enough blood and oxygen. This can happen either because a blood vessel supplying the brain becomes blocked or because a blood vessel bursts, causing bleeding in the brain.
Blocked Blood Vessels
The most common cause of stroke is a blockage in the arteries that supply blood to the brain. This can happen when a blood clot forms in an artery or when fatty deposits called plaque build up and narrow the blood vessels. When blood flow is interrupted, brain cells are deprived of oxygen and nutrients, leading to an ischemic stroke.
Bleeding in the Brain
A stroke can also occur when a blood vessel in the brain ruptures, causing bleeding inside or around the brain. The leaked blood increases pressure on the brain and damages surrounding tissue. Hemorrhagic strokes are often caused by conditions like high blood pressure, aneurysms, or trauma to the head.
What are the Risk Factors?
Certain medical conditions, lifestyle habits, and non-modifiable factors can raise the chances of having a stroke. These include:
- High Blood Pressure: This is the leading risk factor for stroke. Constant pressure on blood vessel walls can weaken them over time, making them more likely to narrow, rupture, or develop clots that block blood flow to the brain.
- Heart and Blood Vessel Conditions: Conditions such as heart disease, irregular heart rhythms, or narrowed arteries can lead to the formation of blood clots. These clots may travel to the brain and block blood supply, triggering a stroke.
- Diabetes: High blood sugar levels can damage blood vessels and affect blood circulation. This damage increases the risk of blockages in the arteries that supply the brain.
- High Cholesterol: Excess cholesterol can build up as plaque inside blood vessels, narrowing them and restricting blood flow. This increases the likelihood of clots forming and causing a stroke.
- Smoking and Alcohol Consumption: Smoking damages blood vessels and reduces oxygen levels in the blood. Excessive alcohol intake can raise blood pressure and increase the risk of bleeding in the brain.
- Obesity and Physical Inactivity: Excess body weight and a lack of regular physical activity can contribute to high blood pressure, diabetes, and heart disease, all of which raise stroke risk.
- Age and Family History: The risk of stroke increases with age. A family history of stroke or heart disease may also raise the likelihood due to shared genetic or lifestyle factors.
What are the Warning Signs and Symptoms of a Stroke?
The symptoms of a stroke usually appear suddenly and can worsen quickly. Key symptoms of a stroke are:
- Sudden weakness or numbness: Weakness, numbness, or paralysis may affect the face, arm, or leg, most often on one side of the body. This can make it difficult to lift an arm, grip objects, or maintain balance.
- Difficulty speaking or understanding speech: Speech may become slurred, slow, or unclear. Some people may struggle to find the right words or have trouble understanding simple sentences.
- Vision problems: Sudden blurred vision, partial loss of vision, or complete loss of sight may occur in one or both eyes. Double vision can also be a warning sign.
- Loss of balance or coordination: Dizziness, difficulty walking, or a sudden loss of coordination may make standing or moving safely difficult.
- Severe headache: A sudden, intense headache with no clear cause can be a sign of a stroke, especially in cases of bleeding in the brain.
- Facial drooping: One side of the face may appear drooped or numb. Smiling may look uneven, with one side not moving properly.
Recognising Stroke Using BE FAST
The BE FAST method helps identify stroke symptoms quickly and highlights the urgency of seeking medical care.
- B – Balance: Sudden loss of balance, dizziness, or trouble walking.
- E – Eyes: Sudden vision problems in one or both eyes.
- F – Face: One side of the face droops or feels numb.
- A – Arms: One arm may feel weak or drift downward when raised.
- S – Speech: Slurred or unclear speech, or difficulty speaking.
- T – Time: Call emergency services immediately and note the exact time the symptoms started, as this information is critical for treatment decisions.
Stroke is a medical emergency. Even if symptoms seem mild or improve, immediate medical attention is essential to reduce the risk of long-term complications.
First Aid and Emergency Response
A stroke is a medical emergency that requires immediate action. The steps taken in the first few minutes can make a significant difference in reducing brain damage and improving recovery. Here is what you should do:
- Call emergency services immediately: If stroke symptoms are noticed, emergency medical help should be contacted without delay. Do not wait to see if the symptoms improve on their own.
- Note the time symptoms began: Knowing when the symptoms first appeared helps doctors decide the most appropriate treatment. This information can be critical in emergency care.
- Keep the person safe and comfortable: The person should be helped to sit or lie down in a safe position. Tight clothing around the neck should be loosened to make breathing easier.
- Do not give food, drink, or medication: Swallowing may be impaired during a stroke, increasing the risk of choking. Medicines should not be given unless advised by medical professionals.
- Monitor breathing and consciousness: If the person becomes unconscious or has difficulty breathing, emergency services should be informed immediately.
- Stay calm and offer reassurance: Remaining calm can help reduce anxiety for the person experiencing the stroke until medical help arrives.
Treatment Options
Stroke treatment focuses on stabilising the patient, preventing further brain damage, and supporting recovery. The approach depends on the type of stroke, the area of the brain affected, and the severity of symptoms:
Medical Management
After the initial emergency phase, treatment centres on managing brain swelling, maintaining healthy blood flow, and preventing complications. Doctors closely monitor vital signs and adjust treatment to support brain function and overall stability. Ongoing medical care helps reduce the risk of worsening symptoms and supports recovery.
Surgical Procedures
Some patients may require surgical or minimally invasive procedures, especially in cases involving bleeding in the brain or significant pressure build-up. These procedures aim to repair damaged blood vessels, relieve pressure on the brain, or prevent further bleeding. The decision depends on the stroke type and the patient’s overall condition.
Interventional Procedures
In certain cases of stroke, doctors may recommend interventional procedures to quickly restore blood flow to the brain and limit permanent damage. These minimally invasive treatments are performed by trained specialists using advanced imaging guidance.
Thrombolysis involves administering clot-dissolving medication to break down the blood clot blocking an artery in the brain. This treatment is most effective when given within a specific time window after the onset of stroke symptoms.
Thrombectomy is a specialised procedure in which the blood clot is physically removed from the blocked artery using thin catheters passed through blood vessels. This approach is used in selected patients with large vessel blockages and can significantly improve outcomes when performed promptly.
The choice of interventional treatment depends on factors such as the type and size of the clot, time since symptom onset, and the patient’s overall medical condition. Early assessment and timely intervention play a crucial role in improving recovery and reducing disability.
Rehabilitation Therapy
Rehabilitation is a key part of stroke treatment and often begins once the patient is medically stable. Therapy focuses on helping regain lost abilities and adapt to any long-term effects. Physical therapy supports movement and strength, speech therapy helps with communication and swallowing issues, and occupational therapy assists with daily activities and independence.
Supportive and Follow-Up Care
Long-term care includes regular follow-ups to monitor recovery progress and address ongoing challenges. Emotional and psychological support may also be needed, as stroke can affect mood, memory, and behaviour. Continued care helps improve quality of life and supports long-term recovery.
Prevention Strategies
Although not all strokes can be prevented, certain steps can significantly reduce the risk as listed below:
- Manage blood pressure: Keeping blood pressure within a healthy range helps reduce strain on blood vessels and lowers the risk of both ischemic and hemorrhagic strokes.
- Control blood sugar levels: Proper management of blood sugar helps prevent damage to blood vessels that can lead to stroke.
- Maintain healthy cholesterol levels: Reducing high cholesterol helps prevent plaque buildup in the arteries, allowing better blood flow to the brain.
- Quit smoking: Smoking damages blood vessels and increases the likelihood of clot formation. Stopping smoking lowers stroke risk over time.
- Limit alcohol intake: Excessive alcohol consumption can raise blood pressure and increase the risk of bleeding in the brain.
- Stay physically active: Regular physical activity supports heart health, improves circulation, and helps maintain a healthy weight.
- Eat a balanced diet: A diet rich in fruits, vegetables, whole grains, and low in unhealthy fats supports overall blood vessel health.
- Attend regular health check-ups: Routine medical check-ups help detect and manage conditions that may increase stroke risk.
Consult a Neurologist/Neurointerventionist at Graphic Era Hospital
Stroke awareness isn’t just about memorizing facts or statistics. It’s about being prepared to protect lives when every second matters. When one person knows the signs, they can help family members, friends, colleagues, or even strangers during a critical moment. Whether there are questions about stroke prevention, concerns about personal risk factors, or a need to discuss a previous stroke experience, our specialists including neurologists at Graphic Era Hospital are here to help. Book a consultation at 1800 889 7351 to receive comprehensive stroke care, from emergency intervention to rehabilitation support.
Frequently Asked Questions (FAQs)
Can a stroke occur during sleep?
Yes, strokes can happen during sleep. Some people wake up with symptoms such as weakness, speech difficulty, or vision problems. This is often called a wake-up stroke and requires immediate medical attention.
Are strokes always painful?
Not all strokes cause pain. Many people experience sudden weakness, confusion, or vision problems without any pain. A severe headache is more commonly linked to bleeding in the brain but does not occur in every case.
Can younger people have a stroke?
Although strokes are more common in older adults, they can also affect younger people. Underlying heart conditions, blood vessel problems, or certain medical disorders can increase the risk at a younger age.
How long does recovery after a stroke usually take?
Recovery varies widely. Some people improve within weeks, while others may take months or longer. The extent of brain damage and how quickly treatment begins play a major role in recovery time.
Can stroke symptoms come and go?
In some cases, symptoms may appear suddenly and then improve. Even if symptoms fade, medical evaluation is essential, as this may signal a serious underlying problem.
Does a stroke always cause permanent disability?
Not always. Many people regain strength, speech, and daily function with proper treatment and rehabilitation. Early care and ongoing therapy greatly influence recovery outcomes.
Can emotional changes occur after a stroke?
Yes, a stroke can affect mood, behaviour, and emotions. Feelings such as anxiety, irritability, or low mood are common and can improve with medical support and counselling.
When should follow-up care begin after hospital discharge?
Follow-up care should begin soon after discharge. Regular check-ups help track recovery, adjust treatment plans, and reduce the risk of future complications.
By Specialities
- Bariatric Surgery
- Cancer Care
- Cardiology
- Dental
- Dermatology
- Diabetes & Endocrinology
- Endocrinology and Diabetes
- ENT (Ear Nose Throat)
- Eye Care
- Gastroenterology
- Haematology
- Health Awareness
- Health Care
- Health Tips
- Hematology
- Hepatology
- Internal Medicine
- Mental Health and Behavioural Sciences
- Metabolic
- Neonatology
- Nephrology
- Neurology
- Nutrition & Dietetics
- Obstetrics & Gynaecology
- Oncology
- Ophthalmology
- Orthopaedics
- Paediatric
- Physiotherapy & Rehabilitation
- Plastic and Reconstructive Surgery
- Psychology
- Pulmonology
- Rheumatology
- Spine
- Urology
Recent Posts
- A Complete Guide to Blood Clots in the Brain
- Heart Attack: Symptoms and Treatment
- World Obesity Day 2026: Understanding, Preventing, and Managing Obesity
- Bacterial and Viral Pneumonia: Causes, Symptoms, and Treatment Options
- World Hearing Day 2026: Empower Yourself to Protect and Improve Your Hearing
Need expert medical advice?
Share your details and our healthcare specialists will reach out to assist you.
By proceeding, you acknowledge and agree to our Privacy Policy, Terms of Use, and Disclaimer.